DIPG Facts
What is the treatment for DIPG?
Surgery
Unlike many brain tumors, a DIPG tumor cannot be removed through surgery. Attempting surgical removal of a brain stem tumor would likely cause severe neurological damage and could even be fatal.
Surgery is not an option for two reasons. First, because the pons is located in the center of the brain, a surgeon could not get to the tumor without damaging the surrounding portions of the brain. Second, if it the tumor could be accessed, total removal would be impossible. A DIPG tumor is not a solid, well-defined mass like some tumors. Instead, the tumor cells spread out between the healthy brain cells. Because the tumor cells could not be entirely removed without also removing the healthy cells, even if surgery were performed, the remaining cells would continue to divide and the tumor would soon return.
Biopsy
A biopsy is a sample of tissue removed from the body for testing. For many tumors, a biopsy is a standard diagnostic tool because it allows the doctors to determine the tumor’s precise characteristics.
Until a few years ago, doctors did not perform a biopsy to diagnose DIPG. They instead diagnosed the disease based solely on a patient’s symptoms and MRI scans. Doctors have not traditionally performed biopsies for two reasons: (1) the risk of causing serious neurological damage was high, and (2) there was little benefit to doing the procedure because the results of the biopsy did not affect how the patient would be treated.
Biopsies are becoming much more common today. The risk that a biopsy will cause neurological damage has been greatly reduced as a result of recent technological advances. As part of a surgical procedure known as a “stereotactic” biopsy, a computer relies on MRI scans of the child’s brain and tumor to guide a thin needle into the tumor to extract cells, while avoiding the critical nerves that run through the pons.
Given their increased safety, stereotactic biopsies have been part of the standard care for DIPG patients in Europe for the past decade. While the practice in the U.S. is moving in this direction, there has been more resistance. The main objection has been from doctors who saw little benefit to the procedure because it would not affect how the DIPG patient would be treated. Given this resistance, doctors in the U.S. now usually perform biopsies only on “atypical” brainstem tumors – those that cannot be clearly identified as a DIPG or a different type of brainstem tumor based on the MRI. In this situation, the biopsy is critical to determining how to treat the patient because, unlike for DIPG, effective treatments are available for other brainstem tumors.
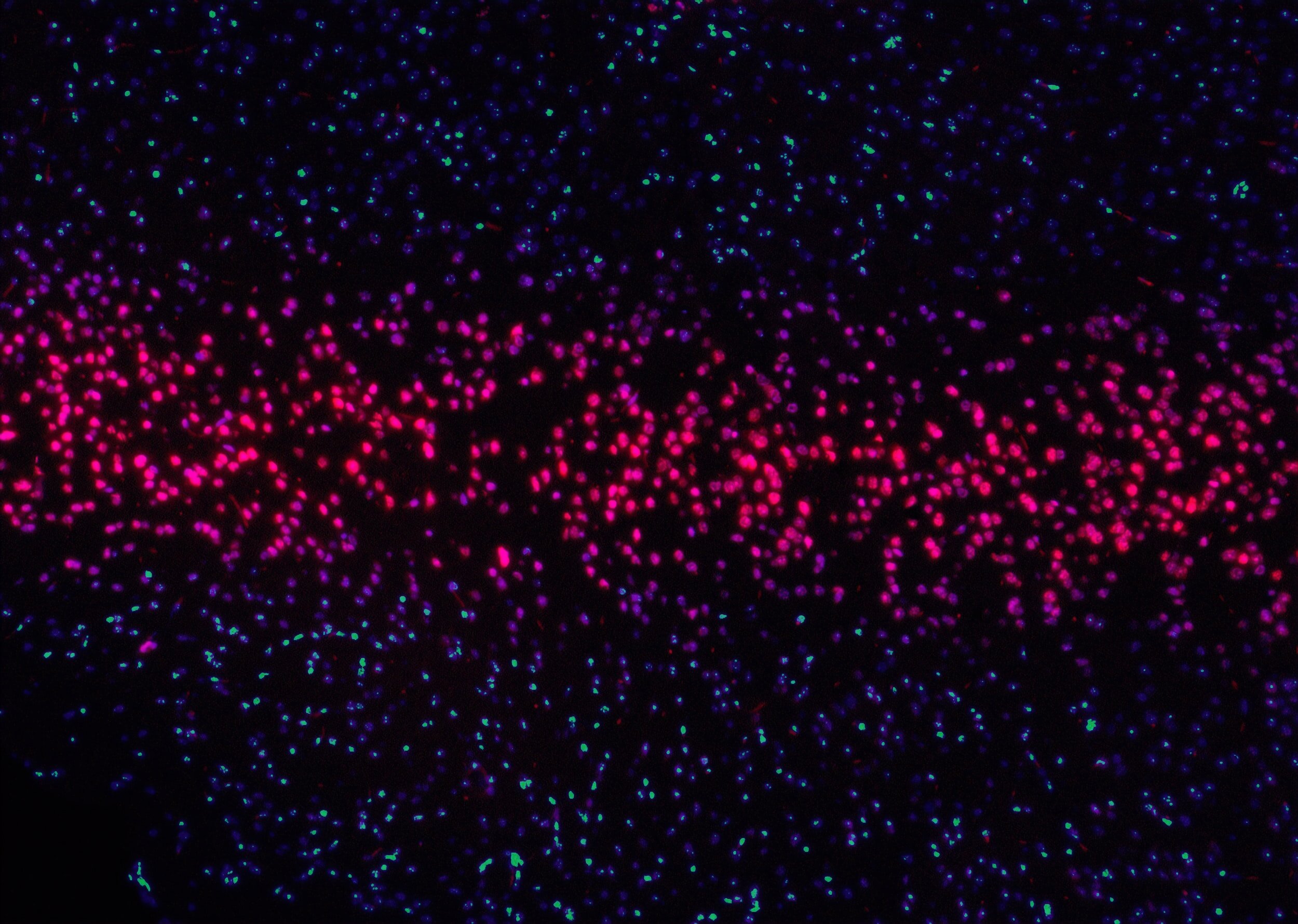
While not all DIPG patients undergo a biopsy in the U.S., biopsies are becoming more common today even for “typical” DIPG tumors. Recent research has shown that not all DIPG tumors are the same. New clinical studies are attempting to personalize the course of treatment for each DIPG patient based on the particular characteristics of each patient’s tumor. Those characteristics can be determined only by performing a biopsy.
As discussed in the Recent Developments section, the increase in biopsies has been a critical factor in the development of our understanding of the biology DIPG tumors.
Radiation
Radiation is part of the standard course of treatment for DIPG patients, as it is the only form of treatment that has proven benefits. For roughly 70% of DIPG patients, radiation causes the tumor to shrink, which provides relief from many of the symptoms associated with DIPG.
The benefits of radiation, however, are only temporary. Even for those patients whose tumors shrink during radiation, the treatment does not increase their chances of survival, and the tumor begins to grow again within months. Because DIPG patients who do not undergo radiation have a median survival length of roughly 5 months, radiation therapy typically extends a patient’s life by about 3 months.
Proton radiation therapy has become popular in recent years for many types of cancer, but most doctors and radiologists do not see a benefit in using this treatment for DIPG tumors. Proton therapy’s primary benefit is that it relies on a proton beam that is more precise than the electron beam used in traditional radiation. This benefit is valuable for solid, well-defined tumors because it allows the radiologist to attack the tumor while sparing the surrounding, healthy cells. This extra precision is not beneficial for DIPG, however. Because a DIPG tumor does not have well-defined edges – the tumor cells spread through the pons, intertwining with the healthy cells – radiation cannot be limit to the solid mass, but instead must extends to the areas around the tumor.
Numerous clinical studies have attempted to improve the effectiveness of radiation by combining radiation with radiosensitizers, which are drugs intended to make cancer cells more likely to die from the radiation. None of the studies so far has shown any benefit to adding a radiosensitizer.
Chemotherapy
In the past 30 years, that have been over 250 clinical trials involving DIPG patients. These trials have involved a wide array of chemotherapy drugs – sometimes alone and sometimes in combination with other drugs. None of these studies has shown any benefit in either the likelihood of survival or the median length of survival.
As discussed in the Recent Developments section, doctors and researchers are actively searching for effective chemotherapy agents. Given the increased understanding of the biology of DIPG tumors, these new approaches can be tailored to the particular characteristics of the DIPG tumor in ways that prior trials could not. These recent developments have given doctors and researchers reasons to be optimistic that they will develop effective treatments for DIPG in the future.
